Every person deserves health and safety, especially throughout their birthing journey. The health of a pregnant person influences not only them personally but also the well-being of their children, family, and communities.
In Missouri, where the maternal mortality rate is the third highest in the nation, health and safety are not universal—this is even more true among Black women, who are three times more likely to die of a pregnancy-related cause during childbirth than white women. BJC HealthCare, with generous support from donors to The Foundation for Barnes-Jewish Hospital, is working to end this disparate cycle and save lives.
PARTNERING TO ELIMINATE HEALTH DISPARITIES
A variety of environmental and social factors, such as socioeconomic status and access to quality health care, influence infant and maternal health outcomes, and a long history of biased public health policies and practices perpetuates the issue. As the largest health care system in Missouri, BJC elevated a systemwide priority to address the root causes of these racially disparate health outcomes and holistically support pregnant people in our communities.
Under the Community Health Improvement (CHI) strategy, BJC is co-designing solutions with neighbors, community organizations, donors, and civic leaders to improve Black infant and maternal health outcomes.  Deidre Griffith, MPH, joined BJC as the vice president of Community Health Improvement in 2023 and leads the systemwide effort to ensure that all people have the opportunity for a healthy, productive life.
Deidre Griffith, MPH, joined BJC as the vice president of Community Health Improvement in 2023 and leads the systemwide effort to ensure that all people have the opportunity for a healthy, productive life.
Thanks to the generosity of donors, The Foundation for Barnes-Jewish Hospital amplifies CHI’s strategy to promote financial well-being, healthy food access, infant and maternal health, and school health and wellness.
“This is home,” Deidre says. “This is our community. We need to do everything we can to remove the social barriers that prevent far too many of our fellow community members, especially racial minorities, from obtaining and maintaining optimal health. We all do better when we all do better.”
Eliminating health disparities will require multiple strategies centered upon the needs and voices of the people directly impacted by those disparities. Strategies include policy change that supports greater access to quality maternal health care, as well as grassroots efforts that empower communities with the tools and resources necessary to be key drivers and influencers of change. Through partnership and collaboration, BJC’s Community Health Improvement is working to build and strengthen relationships that place a premium on transparency, humility, and the provision of culturally responsive, representative, and holistic care throughout the community.
A large-scale transformation, made possible by gifts to the Community Health Improvement Fund at the Foundation, is to build critical care teams reflective of the community and create doula-friendly hospitals. This effort will improve Black infant and maternal health outcomes by ensuring trust and transparency grounded in culturally appropriate, holistic clinical care.
CREATING DOULA-FRIENDLY HOSPITALS
Doulas are non-clinical, trained health care workers who provide physical, emotional, and informational support to pregnant people and their partners throughout the perinatal journey. Evidence demonstrates that community-based doulas influence health outcomes for pregnant people and their infants when integrated into the clinical care space by serving as personal health advocates. In this way, doulas improve the health outcomes and well-being of moms and moms-to-be by reducing Cesarean deliveries, limiting the use of instrument-assisted births, decreasing pre-term and underweight babies, increasing breastfeeding, and reducing maternal and infant mortality.
Community-based doulas are highly trusted allies, especially among people of color, who have experienced direct or indirect disrespect and racism in medical establishments, explains Okunsola Amadou, founder and CEO of Jamaa Birth Village. Okunsola leads doula workshops for BJC clinical care teams, made possible with donor gifts to the Foundation’s Community Health Improvement Fund. Monthly workshops are currently taking place at BJC hospitals Barnes-Jewish Hospital, St. Louis Children’s Hospital, Missouri Baptist Medical Center, and Progress West Hospital. 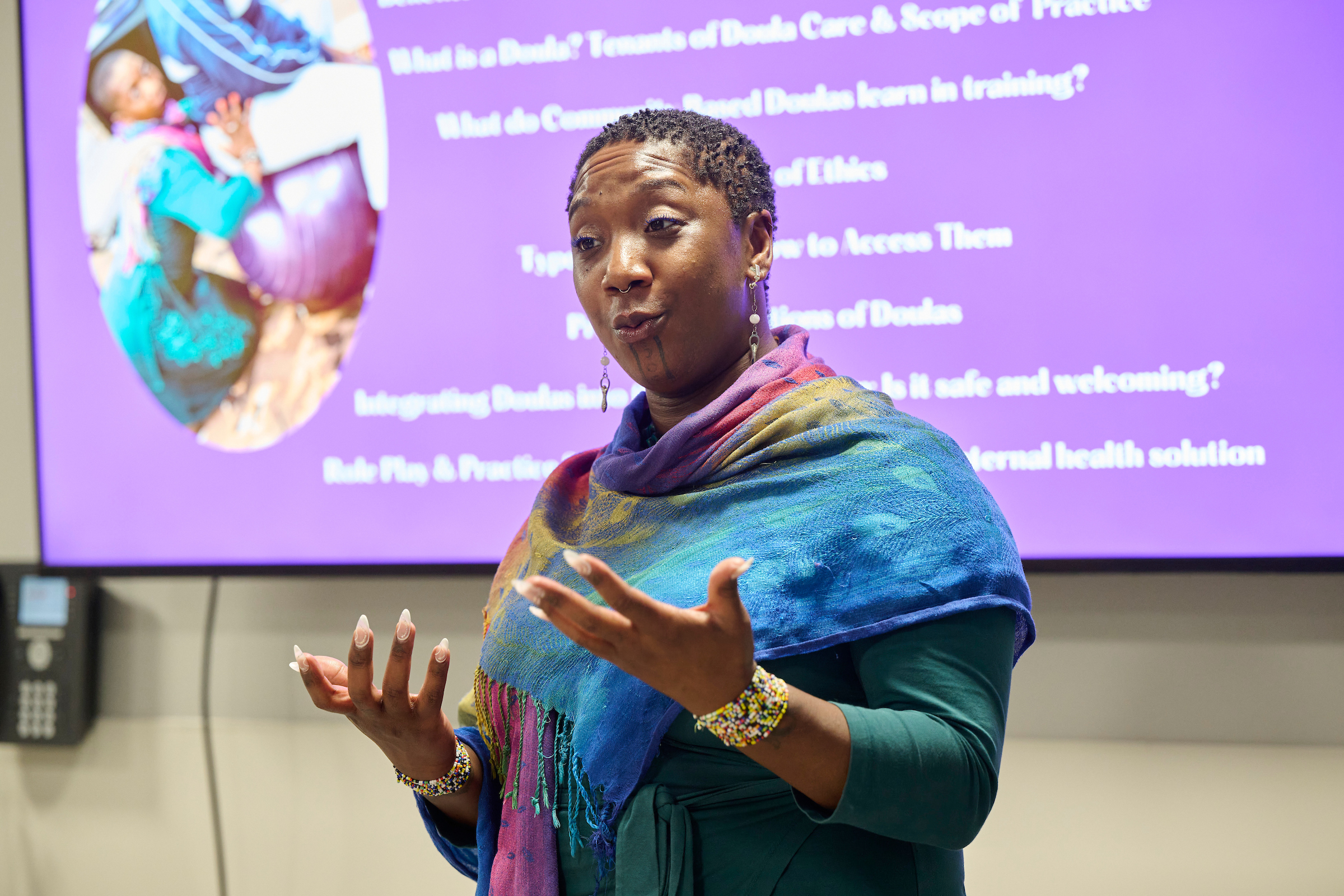
The partnership between Jamaa Birth Village and BJC stems from mutual trust, respect, and authenticity with a shared mission to improve maternal and infant birth outcomes.
“I want to make sure it’s delivered in a way that really makes a cultural shift,” Okunsola says. “To have a hospital trust me to lead their staff members through the workshop to improve patient satisfaction and increase babies thriving … I feel honored that they decided to work with me in this way.”
The workshops are part of BJC’s cultural shift to build doula-friendly hospitals by increasing internal understanding and acceptance of the doula model of care, as well as the historic public health policies that contribute to disparate health outcomes. Together, Okunsola and BJC emphasize that relationships between doulas and clinical care teams are cohesive and supportive of one another.
After attending a doula workshop, Kristin Kelly, BSN, RN, a labor and delivery nurse at Barnes-Jewish Hospital, says her perception of doulas has completely changed. Now, she views them as a true partner to her clinical role.
“It’s changing the way we work in a better way,” Kristin says. “We have great support from our managers and higher-ups to offer this training. This is a continuing education and learning experience with every patient and doula we work with.”
Working in concert, the clinical care team focuses on their clinical responsibilities, such as taking vitals, while the doula provides hyper-focused support and comfort to the birthing person. The labor and delivery clinical care team at Barnes-Jewish Hospital is required to participate in the workshop, though it is also available to any staff. All participants receive a continuing education credit, demonstrating the importance of the workshop.
“Doulas and labor and delivery nurses both desire the best outcome for their patients and will work together to support patients, advocate for them, and meet the wishes of their birth experience,” Kristin says. “When your patient has a doula, you aren’t alone.”

COMMUNITY-CENTERED APPROACH
More than 300 community members connected with BJC clinical care team members and 43 local nonprofit organizations in July at Barnes-Jewish Hospital’s first community baby shower, funded in part by gifts to the Foundation and hosted by the hospital’s Women and Infants Center.
Lashanda Jackson, MSN, RN, women’s health educator and outreach coordinator at Barnes-Jewish Hospital, helped coordinate the event, which celebrated new and expectant families while also connecting attendees to vital community resources. Leveraging its brand recognition, BJC amplified its community partners and facilitated meaningful connections among new and expectant families at the event.
“We’re getting behind our community-based doula partners by spreading the word about the awesome things they’re doing in the community and making sure we’re being supportive of that with our voice,” LaShanda says.
Additional topics at the baby shower event included infant safe sleep, car seat safety, nutrition in pregnancy and lactation, maternal mental health wellness and care, maternal warning signs, and breastfeeding support—all of which increase maternal and infant health while also building relationships in the community. In a post-event survey, most participants stated meeting with community-based doulas was the most useful aspect of the event.
SCALABLE AND GENERATIONAL HEALTH EQUITY
This ongoing effort within BJC and with the community to improve health outcomes of pregnant people and their families relies on authentic relationships, collaborations, and listening every step of the way.
“We’re staying present and transparent through bidirectional communications with community partners,” Deidre says. “We’re building trust with our community partners, and we’re learning what they need right alongside them. It’s a continuous evolution.”
BJC and the Foundation will continue to employ a community-centered approach with philanthropic support to enact long-term strategies, including:
- Train BJC clinical care teams and patients on the doula model of care through workshops to improve knowledge and acceptance of doulas, as well as train individuals interested in becoming community doulas.
- Connect pregnant people in under-resourced communities with doulas to support positive long-term health outcomes for Black pregnant people and their babies.
- Evaluate and change hospital policies and practices that may exacerbate health inequities and health outcomes using community input.
- Advocate for doula reimbursement through Medicaid to scale impact statewide while also partnering with donors to create a fund at the Foundation to support at least 50 pregnant people in the coming year who could not otherwise afford access.
“We do still have a barrier with doula access because there is currently no third-party payer coverage or other sustainable sort of source of funding,” LaShanda says, adding that many of the patients in the obstetric clinic at Barnes-Jewish Hospital are Medicaid-eligible, though even insurance doesn’t cover a doula. “The place where we really want to be is where any mom or mom-to-be can walk through our hospital doors and say, ‘Hey, I need support,’ and we can connect them with a doula without a financial barrier for the patient.”
Several states across the country have partnered with private and public stakeholders to develop sustainable mechanisms to reimburse doulas through Medicaid. BJC is working to add Missouri to this list by demonstrating the value and impact doulas have for Missouri families.
Currently, BJC Community Health Improvement and the Foundation are building strong relationships with community-based doulas and are working to establish a doula provider fund that offsets the cost of providing a doula to patients from the pre-natal to post-partum period.
In addition to Jamaa Birth Village, Barnes-Jewish Hospital connects patients to doulas through relationships with the St. Louis Doulas of Color Collective (an initiative of Jamaa Birth Village); St. Louis Doula Project; Doula Love, Light & Life, LLC; and Parents as Teachers National, many of which participated in the community baby shower and met with families.
Deidre is excited about the opportunity to try unique collaborations and approaches focused on eliminating health disparities.
“Philanthropic gifts support hospitals in their pursuit of creativity and innovation in addressing health inequities and community health improvement,” she says. “These gifts enhance our ability to go beyond the status quo to do something that could have deeper, longer-term, and sustained impact on patient and community health, especially in terms of prevention.”
Charitable gifts from individuals, families, organizations, and corporations help bring these strategies to life and lay the foundation for transformative system change.
“Large-scale impact takes time, and it is time worth taking to ensure that every person has the healthy and safe birthing experience they deserve,” Deidre says.
EARLY INTERVENTION FOR HIGH-RISK PREGNANCIES
A concerning risk during pregnancy to both the birthing person and child is high blood pressure. With generosity and visionary support from donors Charles and Rosalyn Lowenhaupt, Barnes-Jewish Hospital provides battery-operated blood pressure cuffs for pregnant patients to monitor their health safely at home. In 2022, 200 patients Lowenhaupt received the cuffs. The monitors help patients and their care teams look for signs of serious pregnancy complications, such as preeclampsia, and enable early intervention and management with communications and reminders to patients via text.
Hospital provides battery-operated blood pressure cuffs for pregnant patients to monitor their health safely at home. In 2022, 200 patients Lowenhaupt received the cuffs. The monitors help patients and their care teams look for signs of serious pregnancy complications, such as preeclampsia, and enable early intervention and management with communications and reminders to patients via text.
Under the leadership of Denise Willers, MD, a Washington University obstetric and gynecologic specialist at Barnes-Jewish Hospital, the Outpatient Blood Pressure Cuff program expanded in 2022 to include postpartum patients who experienced hypertensive disorders of pregnancy (HDoP). This group accounts for about 15% of the patient population, compared to 5% nationally. Women of color from low-income households disproportionately experienced HDoP and are more vulnerable to higher rates of readmission and severe maternal morbidity after delivering their babies.
One participant in the program says, “I had an emergency situation where I had to come and get blood pressure medication immediately. The text message program helped nurses identify that there was an issue that I would’ve otherwise missed.”
Through their gift to The Foundation for Barnes-Jewish Hospital, the Lowenhaupt family has made it possible to sustainably meet this critical need to prioritize and improve maternal health.
Give Now & Support Infant and Maternal Health